LUQ pain and collapse
A 41yo man collapsed at triage.
He was ashen, complaining of LUQ and lower rib pain. He denied trauma, travel or immobilisation. He had no infective symptoms.
The pain had been present a few hours.
PMHx was IVDU and previous IE with tissue MVR, not anticoagulated.
His obs: HR 110, BP 80/ sats 100, afebrile
He was tender in the LUQ and epigastrium. HS dual and nil. chest clear.
IV fluid bolus and autotransfusion led to a BP 110/ and HR 110.
EFAST at the bedside revealed:
RUQ (annotated below)
LUQ (annotated below)
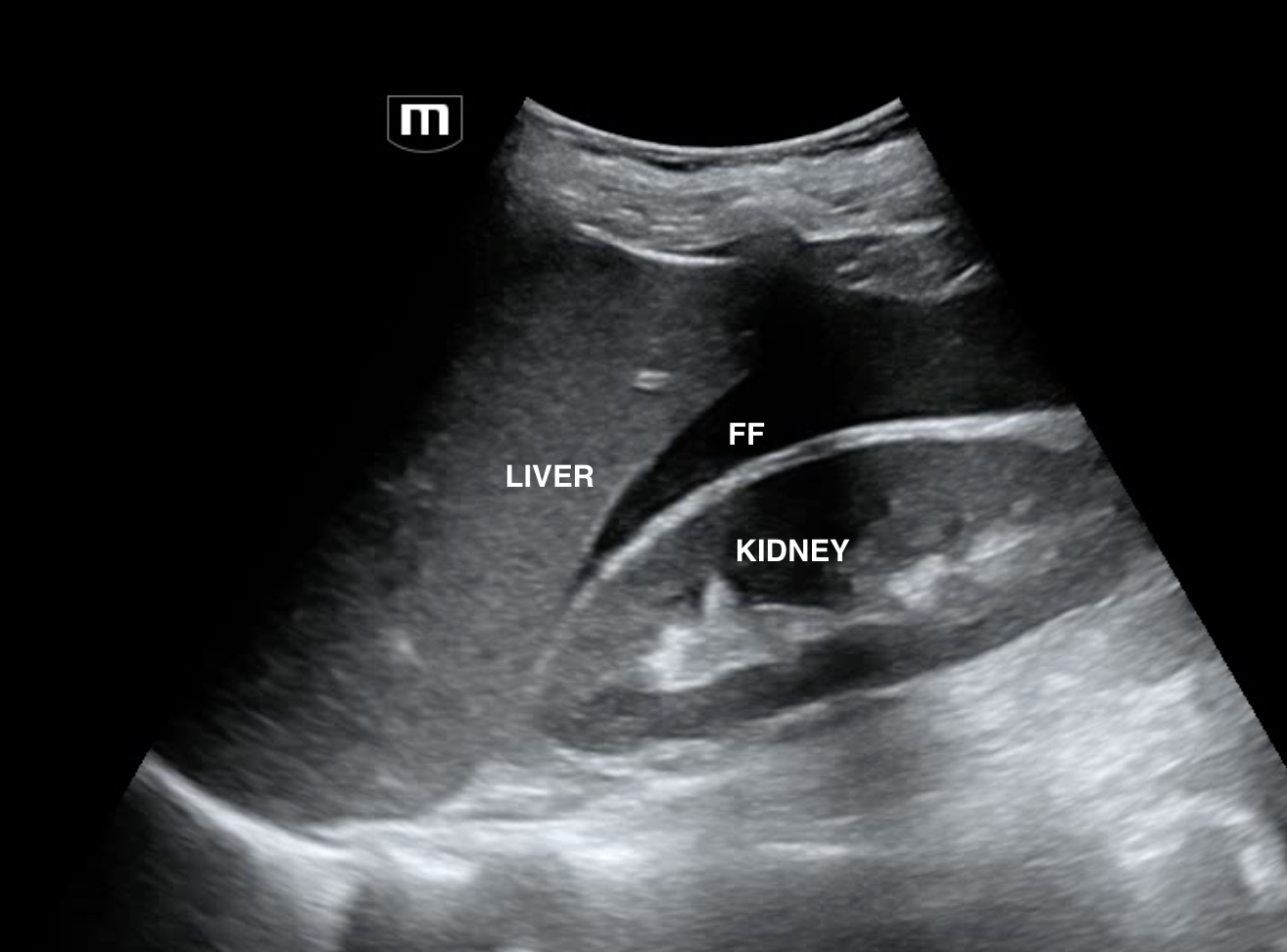
RUQ (annotated)
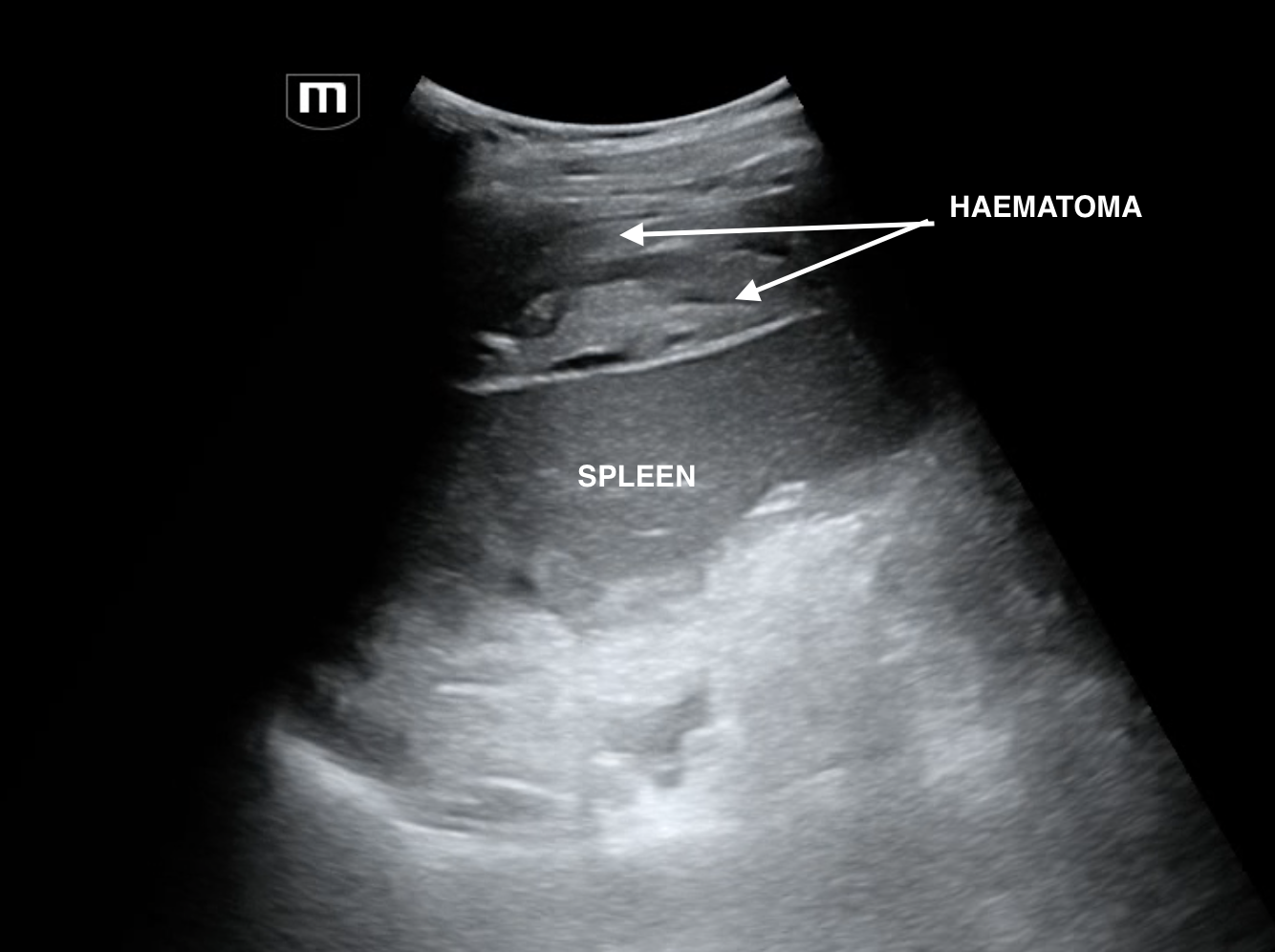
LUQ annotated
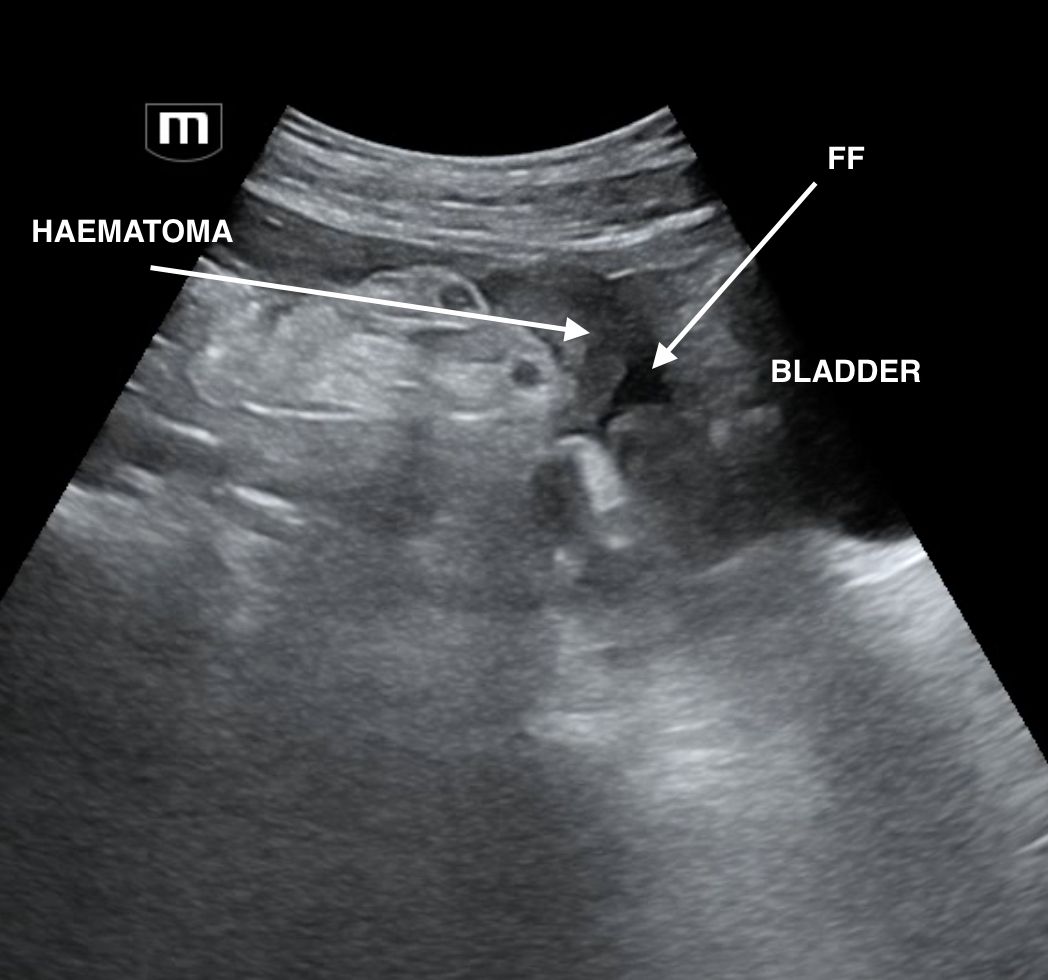
Pelvis long (annotated)
Given the patient's hx of IVDU, we wondered whether the FF could have been due to chronic liver disease, ascites and associated sepsis. Pancreatitis was another differential. The hypoechoic material layering around the spleen raises the question of primary peritoneal malignancy like mesothelioma. But how likely is that?
More worrying for us with a normal liver and the layering hypoechoic material was intraperitoneal bleeding. DDx intraabdominal artery aneurysm rupture eg splenic/ SMA/ renal, liver HCC bleeding, splenic rupture.
A quick check revealed a normal aorta.
CT abdo was expedited and a MEP pack was requested.
CT abdo revealed a dilated splenic artery probably secondary to previous mycotic aneurysm which had ruptures. Pt went to IR and had an uneventful recovery.
