Syncope
A 22yo female was brought into ED post syncopal episode while visiting a relative on the ward.
The relative was having an IV placed. The patient felt sick, walked out of the room and lowered herself to the floor. She had a PHx of one faint post heavy period, otherwise nil else.
OE
HR 58, BP 97/58 sats 100 afebrile
Examination was unremarkable.
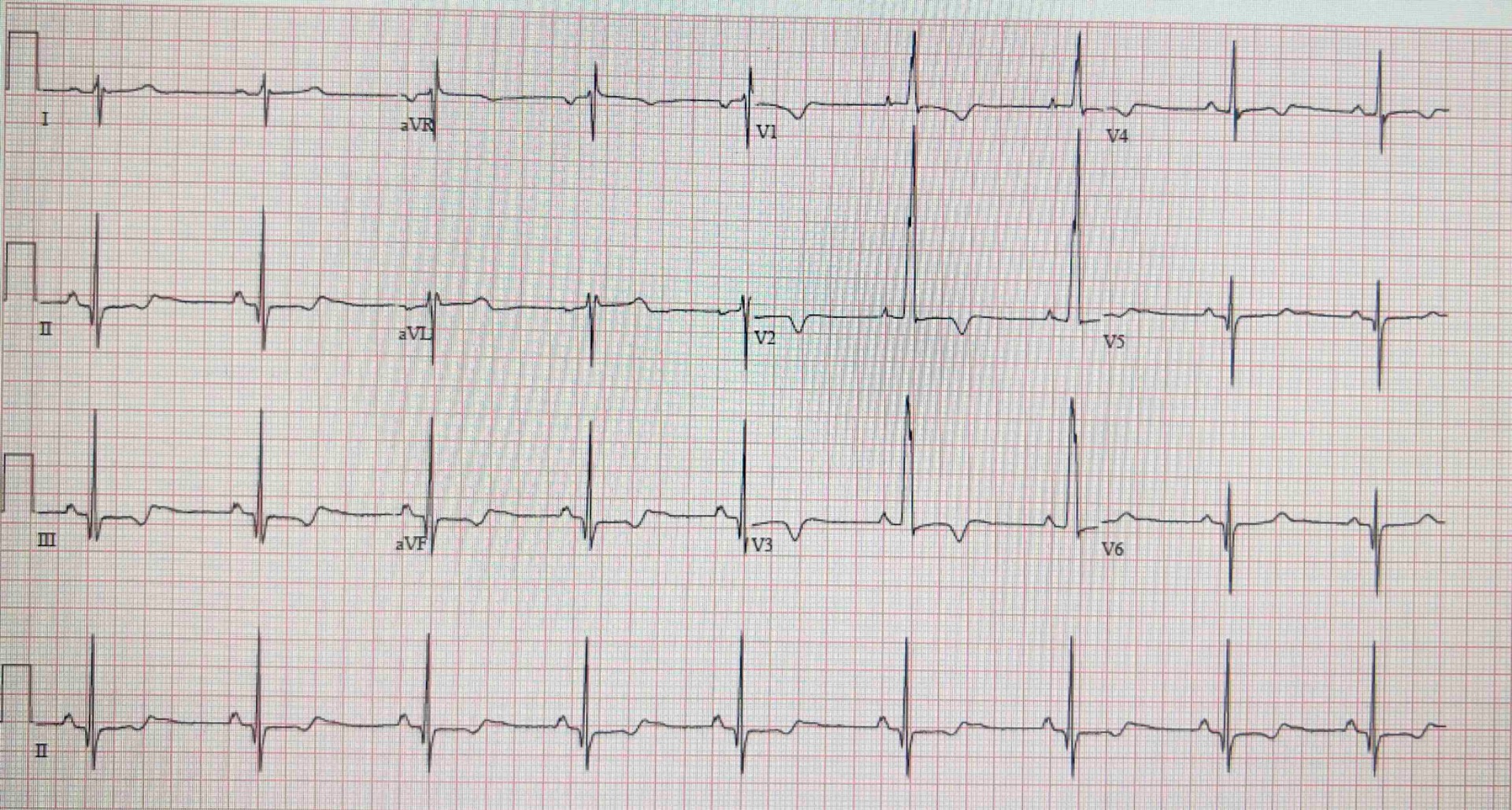
ECG:
troponin and d dimer were negative.
Bedside US revealed
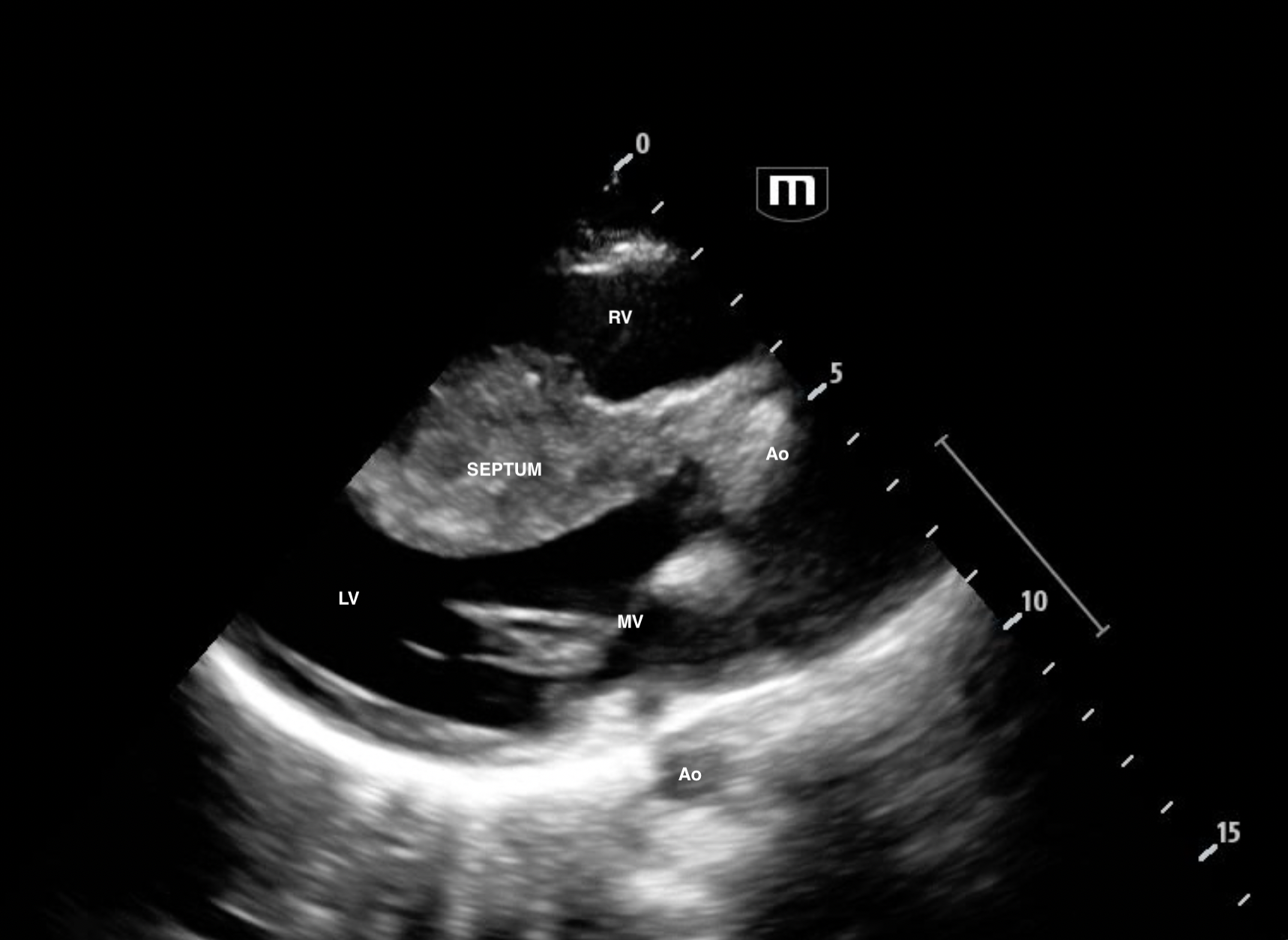
PLAx
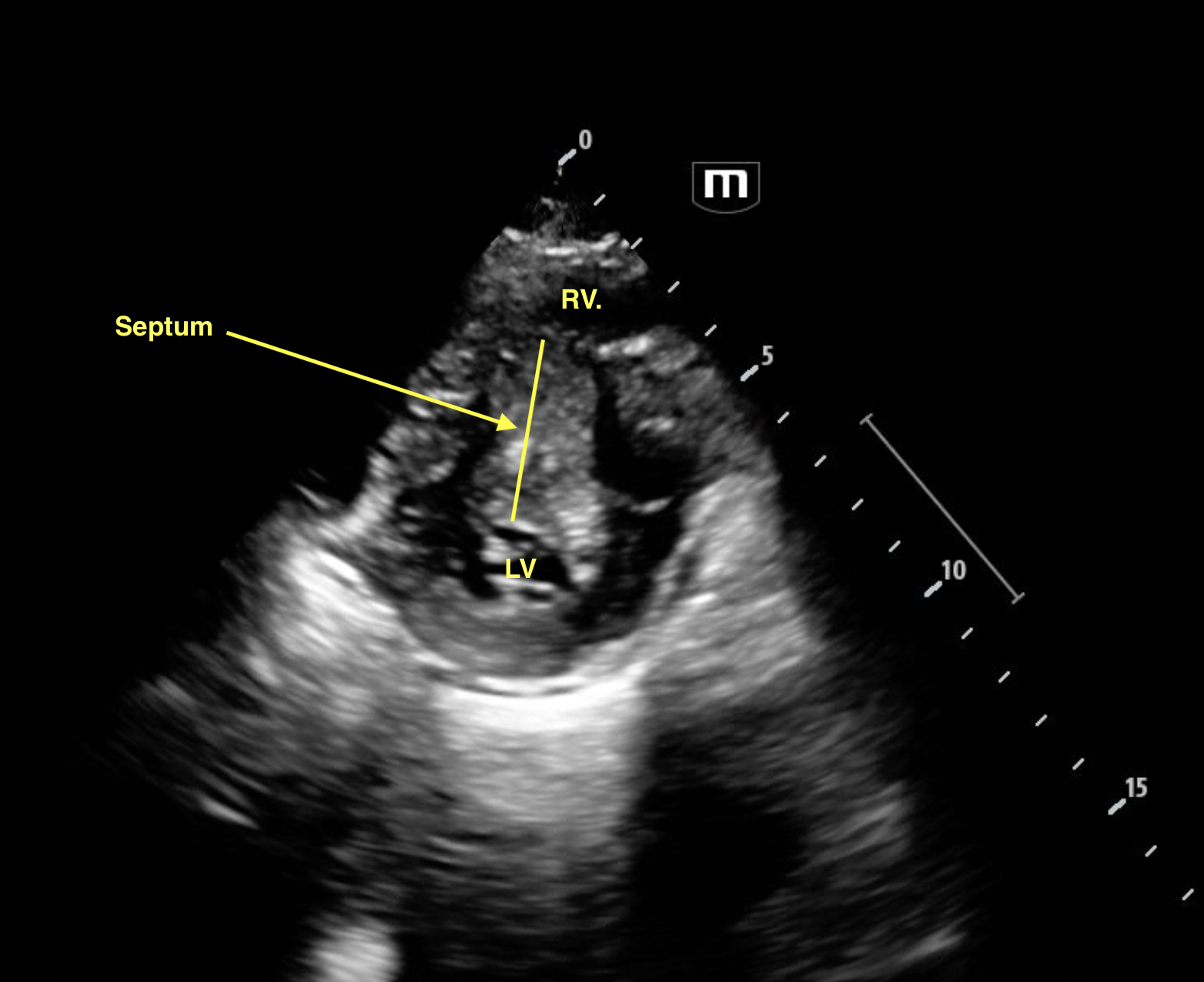
PSAx
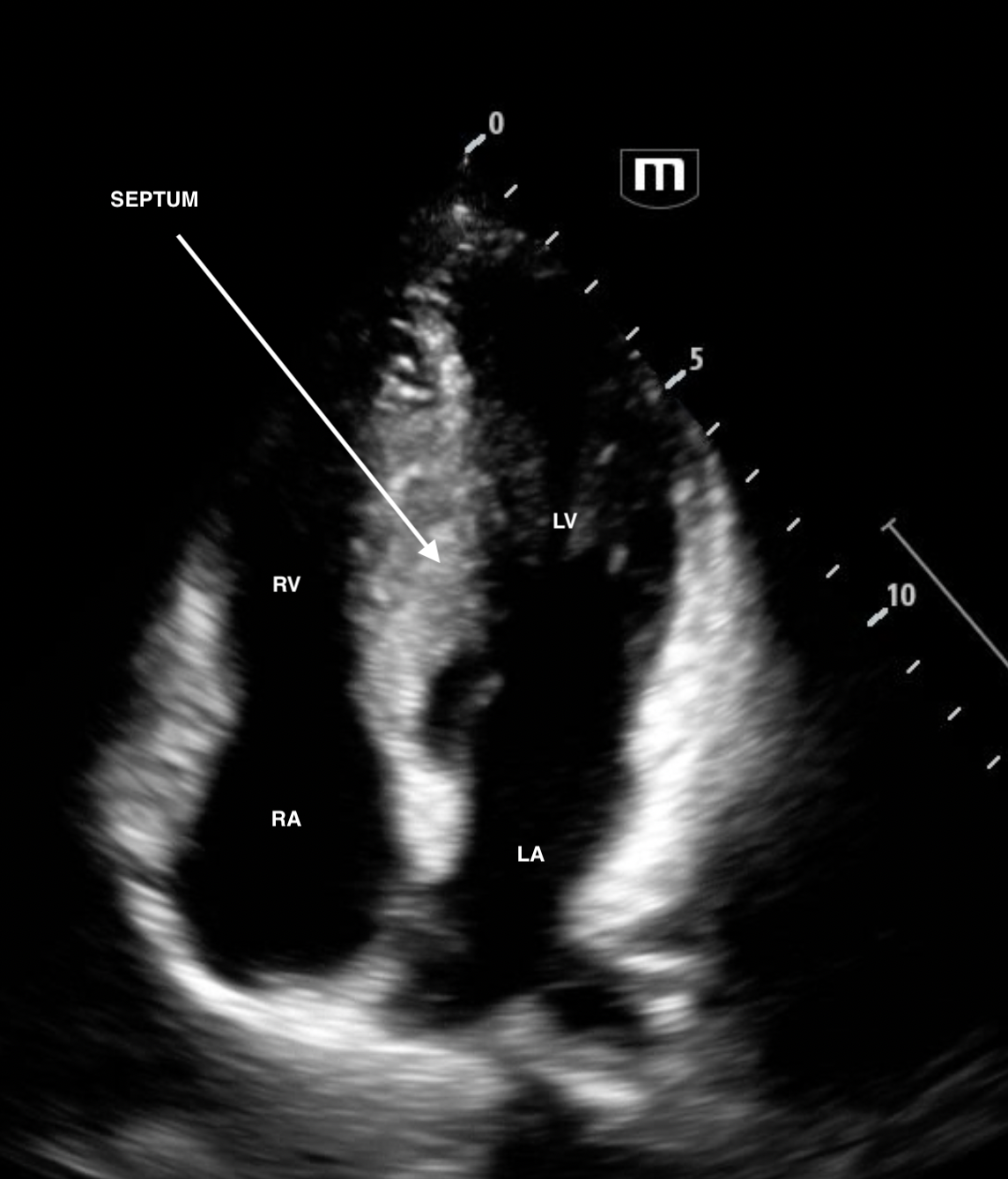
A4C
The patient was admitted to cardiology. Formal echo revealed septal thickness of 3.2cm (normal <1cm). RV inflow was turbulent with a Vmax 4.2m/s (!!!!!!!) Mean 30mmHg and Peak Gradient of 69mmHg. For context, normal RV inflow ie flow across the tricuspid valve has a Vmax <0.7m/s.
The high Vmax shows that there is obstructed flow across the TV: acting like a tricuspid stenosis. This leads to impaired RV filling. Hence the patient's syncope with the vagal episode or with acute volume loss.
Typically septal hypertrophy affects the LV side of the septum. But in this case, it's bulging into the RV.
Patient was diagnosed with HOCM and booked into the cardiac genetic clinic.
